
First Health PPO Network For Visitors Insurance
First Health Network is a popular PPO health network available in some of the top-rated visitor insurance plans.
When you buy visitor’s insurance for the USA, basically you are buying short-term health insurance for the duration of your stay in the United States.
Some travelers may be familiar with the term PPO, but if you are not and you need more information, then, let us understand more about PPO and the First Health PPO Network.
What Is A PPO Health Network?
What is a PPO Network? In the U.S. PPO network refers to the Preferred Provider Organizer having contracts with medical providers such as hospitals, clinics, pharmacists, laboratories, and other healthcare providers.
These providers have contracts with third-party insurance providers who provide healthcare facilities at a reduced rate to the insurance provider’s clients or members.
Some of the largest PPO networks in the USA are:
- United Healthcare PPO
- First Health Network PPO
- PHCS Health Network
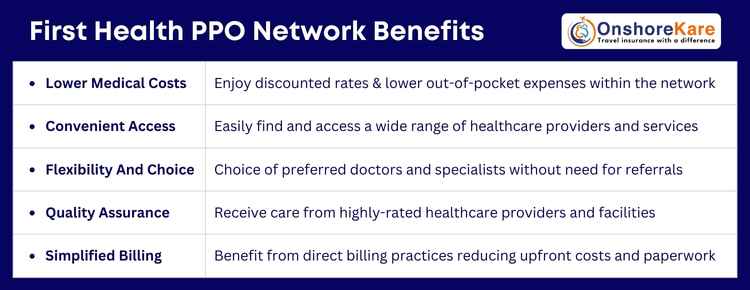
Why Use PPO Network?
The policy provides better-discounted rates for medical treatment and services availed within the network.
Visitor insurance plans offer the benefit of using In-Network and Out-of-Network Doctors and Hospitals for treatment. The key benefit to the insured is lower out-of-pocket expenses within a Health Network.
What Is First Health PPO Network?
The first health PPO network is a Preferred Provider Organization (PPO) that offers a wide range of healthcare services through a network of preferred healthcare providers and facilities.
It is designed to provide members with access to high-quality medical care while offering cost savings through negotiated rates with healthcare facilities.
Key Features Of First Health PPO Network:
Extensive Network providers:
- Includes a broad range of healthcare providers, including primary care physicians, specialists, hospitals, other healthcare facilities, and health care professionals.
- Offers access to thousands of healthcare providers nationwide, ensuring members can find care close to home while traveling.
Cost Savings:
- Members benefit from negotiated rates with in-network providers, which are lower than standard rates.
- Reduced out-of-pocket costs through lower copays and insurance when using in-network providers.
- They consistently provide optimal cost for treatments and procedures
Flexibility:
- Allows members to choose their healthcare providers, offering the flexibility to see any provider within the network without the need for referrals.
- Members can also see out-of-network providers, although at higher out-of-pocket costs.
Direct Billing:
- Many in-network providers offer direct billing to the insurance company, reducing the need for members to pay upfront and seek reimbursement.
Quality Care:
- The network includes many highly-rated healthcare providers and facilities, ensuring members receive quality care.
- Regular assessments and evaluations of network providers help maintain high standards of care.
Comprehensive Services:
- Covers a wide range of medical services, including preventive care, emergency services, specialist care, hospital stays, and more.
- Includes coverage for various medical needs, from routine check-ups to complex medical treatments.
Accessibility:
- User-friendly online tools and resources to help members locate providers, check benefits, and manage their healthcare needs.
- Customer service support to assist members with any questions or issues related to their healthcare coverage.
Find A Provider In The First Health PPO Network
The First Health PPO Network has in its network more than:
- 868,000 Providers
- 695,000 healthcare professionals
- 5,000 plus Hospitals
- 110,000 plus ancillaries
First Health PPO Network collaborates with national insurance carriers to enhance its provider network and offer comprehensive coverage.
To locate a First Health PPO Provider Visit: https://www.myfirsthealth.com/
If you have a visitors’ insurance plan that includes coverage through the First Health PPO network, you can locate participating providers by visiting the First Health Group Corp website.
Using First Health PPO Network With Visitors Insurance Plan

While using your First Health PPO Network keep these things in mind:
When you contact a medical provider or present your ID card, please indicate the PPO Network when you have to use the insurance. Explain by saying something like:
- “My Insurance uses the First Health PPO network and I found your details on the First Health PPO network search”
- It is advisable to avoid saying: “I have XYZ Insurance” or “I have XYZ Plan”
Providers might not be aware of all the visitor insurance plans but they are familiar with the Networks. Using network services can help you reduce medical expenses.
If your insurance plan provides First Health PPO Network access, you can better manage your healthcare expenses and ensure a smoother experience when seeking medical care.
History And Background Of First Health PPO Network
To offer affordable healthcare solutions to patients across the U.S. First Health was founded as a subsidiary of Coventry Health Care Inc. in the year 1985.
Later it was acquired by Aetna Health Inc. which improved offerings and expanded the network reach of First Health PPO Network
Conclusion
Visitors Insurance with health network access is a good choice and First Health Network is a premier national network that consistently provides optimal cost and care outcomes for its members.
The network is a wholly owned subsidiary of Aetna Inc. and has been recognized for its quality and extensive provider network.
Frequently Asked Questions
What Is First Health PPO?
First Health Network is a major PPO network with over 1 million providers in the United States. The network collaborates with regional health plans to offer flexible and comprehensive coverage. The network provides access to a wide range of health providers and facilities. First Health is a popular choice for patients seeking quality healthcare.
Is First Health A Part Of Aetna?
- The First Health Network has been owned by Aetna, Inc. since 2013.
- Aetna is a well-known health insurance company.
- First Health is a part of Aetna’s network of health insurance providers.
What Is A PPO Network?
PPO or preferred provider organization is a network of many established highly qualified medical practitioners and well-recognized hospitals in the USA, known as the PPO Network.
In short Preferred Provider Organization (PPO) is a type of health plan that contracts with medical providers, such as hospitals and doctors, to create a network of participating providers
Why Use A PPO Network?
The policy provides better-discounted rates for medical treatment and services availed in the network
What Are Provider Networks?
Provider networks are networks of Hospitals, Doctors, and other healthcare providers and facilities who have agreed to offer services to insured persons (of certain medical plans) at negotiated rates. These rates are negotiated with the insurance provider’s office and passed on to plan holders of the respective providers.
What Is National Provider Identifier (NPI) information
The National Provider Identifier (NPI) is a unique 10-digit identification number issued to healthcare providers in the United States by the Centers for Medicare and Medicaid Services (CMS)


