The Claim Process for Travel Insurance Plans: What to Expect and How to Prepare
Filing a travel insurance claim feels stressful not because the rules are unclear, but because claims are usually triggered during already difficult situations. Medical emergencies, trip disruptions, and unexpected expenses leave little room for delay, confusion, or trial-and-error decision making.
This guide explains how the travel insurance claims process actually works in practice: what happens at each stage, which factors most directly influence claim timelines, and why some claims move forward smoothly while others slow down. It is written for travelers and families who want clarity before a claim is needed, not after problems begin.
The focus here is not on policy features, marketing language, or fine print. It is on real-world claim outcomes and the specific actions that reduce uncertainty, minimize back-and-forth, and improve the likelihood of a predictable claim experience.
Quick Answer: Is the Travel Insurance Claims Process Complicated?
The travel insurance claims process is not complicated when three conditions are met: the incident is reported promptly, treatment is taken at an appropriate facility, and documentation is complete. In these situations, claims generally move forward with limited follow-up and predictable timelines.
The process becomes complicated when any of these conditions are missed. Delayed notification, treatment outside the insurer’s network, or incomplete or unclear documents increase coordination effort and extend processing time. International claims often involve multiple medical providers, currencies, and billing systems, which adds complexity if expectations are not set early.
In most cases, claim delays are not the result of insurers refusing valid claims. They occur because of gaps in communication, documentation, or process timing. Knowing what actions to take at the right moment has a direct and measurable impact on how smoothly a claim progresses.
What Determines Whether a Travel Insurance Claim Moves Smoothly
Most smooth travel insurance claims share three common factors:
- Early notification to the insurer or assistance team
- Treatment at an in-network healthcare provider, whenever possible
- Complete and clearly organized documentation
When any one of these factors is missing, claim timelines typically extend and follow-up requests increase.
Quick Travel Insurance Claim Readiness Check (Self-Assessment)
This short self-check helps identify potential gaps before travel. It is not a test, and there are no right or wrong answers. The goal is to understand whether you are prepared to navigate a travel insurance claim if an unexpected situation arises.
Claim Readiness Questions
- Do you know how to contact your insurer’s assistance or emergency support team while travelling?
- Yes, the contact details are saved and easily accessible
- I know where to find them if needed
- No, I’m not sure how to reach them
- Do you understand whether your travel insurance plan supports cashless treatment, reimbursement, or both?
- Yes, I understand how my plan works
- I have a general idea but am not fully sure
- No, I’m unclear on the difference
- If medical care is needed, do you know how to identify an in-network hospital or provider?
- Yes, I know how to check or whom to contact
- I would need help from the insurer
- No, I wouldn’t know how to check
- Are you able to store or photograph bills, medical reports, and receipts while travelling?
- Yes, I can capture and store documents digitally
- Possibly, but not consistently
- No, I rely on physical paperwork only
- Do you know when you are expected to notify the insurer after a medical incident or covered event?
- Yes, I understand the timing expectations
- I’m not completely sure
- No, I don’t know
How to Interpret This Self-Check
If you selected “not sure,” “unclear,” or “no” for one or more questions, it does not mean a claim will fail. It does indicate areas where lack of preparation can lead to delays, additional follow-ups, or unnecessary stress during an emergency.
Addressing these gaps before travel helps ensure smoother coordination and more predictable claim outcomes.
Key Takeaways to Understand Before You File a Travel Insurance Claim
- Claims move more smoothly when incidents are reported early and coordinated through the insurer’s assistance team.
- Using in-network hospitals, when possible, significantly reduces paperwork and out-of-pocket expenses.
- Cashless and reimbursement claims follow different processes and timelines, and should not be assumed to work the same way.
- Complete and accurate documentation has the greatest impact on claim review speed and resolution.
- Most claim delays are caused by missing or unclear information, not by insurers rejecting valid claims.
- Understanding how the claims process works before travel reduces stress and decision-making pressure during emergencies.
Why Travel Insurance Claims Feel Confusing
Travel insurance claims often feel confusing because the process involves more parties than just the insurer. Medical providers, hospital billing teams, assistance companies, and third-party administrators may all be involved, particularly when treatment occurs outside the traveler’s home country.
A single medical visit can generate multiple bills from different providers, each following its own billing, coding, and documentation standards. When differences in healthcare systems, currencies, and timelines are added, even valid claims can take time to reconcile. This complexity increases further when travelers are unfamiliar with provider networks or delay notifying the insurer.
In most cases, confusion arises from limited visibility into how these moving parts interact, not because the claims process is intentionally complicated. Understanding this early helps set realistic expectations and reduces frustration when follow-ups are required.
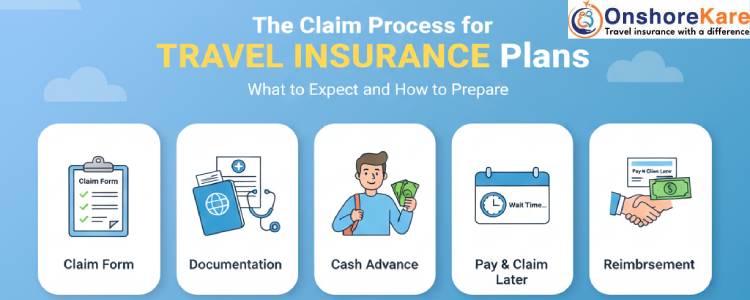
How the Travel Insurance Claims Process Works
Understanding the travel insurance claims process step by step helps set realistic expectations and reduces avoidable delays.
Step 1: A Medical Emergency or Covered Incident Occurs
The first priority is always medical care or personal safety. Once the situation is stable, the insurer’s assistance or claims support team should be contacted as soon as possible. Early notification allows the insurer to document the incident from the start, guide next steps, and suggest appropriate facilities when needed.
Delaying notification can limit available options later, particularly for cashless treatment or coordinated care.
Do this: Contact the insurer or assistance team as soon as the situation is stable.
Avoid this: Waiting until hospital discharge or return from travel to report the incident.
Step 2: In-Network vs Out-of-Network Treatment
Most travel insurance plans operate through a preferred provider network. Visiting an in-network hospital usually results in lower upfront payments and simpler billing, as the hospital can coordinate directly with the insurer.
When possible, receiving treatment within the insurer’s network significantly reduces paperwork and out-of-pocket expenses. Out-of-network treatment is still permitted, but it often requires the traveler to pay expenses upfront and seek reimbursement later. This increases documentation requirements and can extend processing timelines.
Do this: Ask the assistance team to help identify an in-network facility when feasible.
Avoid this: Choosing a provider without checking network status unless the situation is an emergency.
Step 3: Cashless Claims vs Reimbursement Claims
Cashless claims allow the insurer to settle eligible medical expenses directly with the healthcare provider, subject to approvals and policy limits. These arrangements typically require advance coordination and clear communication between the hospital and insurer.
Reimbursement claims require the traveler to pay expenses first and submit supporting documents afterward. While common, this process depends heavily on accurate medical reports, itemized bills, and proof of payment, making attention to detail essential.
Do this: Confirm whether cashless treatment is available before admission.
Avoid this: Assuming all hospitals automatically offer cashless arrangements.
Important Note on Cashless Treatment
Cashless treatment does not mean automatic approval. It depends on provider network status, policy terms, coverage limits, and timely coordination between the healthcare provider and the insurer. Even when cashless arrangements are available, documentation and eligibility requirements still apply.
Step 4: Claim Submission and Review
Once treatment or the covered incident is complete, claim forms and supporting documents are submitted for review. Insurers verify eligibility, coverage limits, and documentation consistency before approving payment.
Processing timelines vary based on claim complexity and the completeness of submitted information. Follow-ups are most often required when documents are missing or unclear, which is why organized documentation plays a critical role.
Do this: Submit all required documents together and respond promptly to clarification requests.
Avoid this: Sending partial information in multiple submissions unless specifically requested.
What Insurers Typically Review First in a Travel Insurance Claim
When a claim is submitted, insurers usually begin by verifying a small set of core details before reviewing expenses in depth.
- Whether the policy was active on the date of the incident
- Whether notification timelines were followed
- Whether the treatment or expense aligns with the type of coverage purchased
- Whether submitted documentation supports the claimed expenses
Clarifying these points early helps prevent avoidable follow-ups and sets realistic expectations during claim review.
Documents You Must Keep For Travel Insurance Claims (And Why They Matter)
Missing documents do not usually result in claim rejection, but they almost always lead to delays in claim processing and payouts. Documentation is the backbone of any travel insurance claim, and incomplete or unclear paperwork is the most common reason otherwise eligible claims slow down.
Medical documents such as doctor’s notes, diagnosis reports, discharge summaries, and itemized bills explain what treatment was provided and why. Insurers rely on these records to verify that expenses align with policy coverage.
Travel documents, including passport copies, visa pages, travel tickets, and policy details, establish who is covered and during what period. Proof of payment, such as receipts or bank statements, confirms that expenses were actually incurred.
In certain situations, additional documentation may be required. Police reports are commonly needed for theft or loss claims, while airline confirmations are often required for baggage or trip delay claims. Keeping digital copies of all documents makes submission, clarification, and follow-up significantly easier.
Common Reasons Travel Insurance Claims Get Delayed or Denied
Most travel insurance claim issues are not caused by ineligibility, but by process gaps. Understanding where claims commonly slow down or fail helps avoid unnecessary complications.
Claims are frequently delayed when incidents are reported late, documentation is incomplete, or treatment is taken outside the insurer’s network without prior notification. Inconsistent billing details or missing medical explanations can also extend review timelines.
Claim denials usually occur when expenses fall outside policy coverage, exceed benefit limits, or relate to exclusions clearly stated in the policy. These outcomes are typically tied to coverage boundaries rather than errors in claim submission.
Reviewing coverage limits and exclusions in advance helps prevent misunderstandings during claim review. Assuming that all medical expenses are covered regardless of circumstances often leads to frustration later.
What Are Special Travel Insurance Claim Situations to Be Aware Of?
Certain types of travel insurance claims require extra attention because they involve additional documentation, third-party confirmation, or different evaluation criteria.
Trip cancellation or trip delay claims typically depend on clearly defined covered reasons and supporting proof from airlines or travel providers. Lost or delayed baggage claims usually require reports to be filed with the airline before an insurance claim can be reviewed.
Medical claims may also be assessed differently depending on whether they involve accidents or illnesses. Understanding these distinctions helps ensure that the correct medical information is submitted from the outset.
Collecting supporting documents at the time of the incident makes claim submission significantly smoother. Attempting to obtain reports or confirmations after returning home often results in missing or incomplete information.
How Long Do Travel Insurance Claims Usually Take To Settle
Travel insurance claim timelines vary based on claim complexity and the completeness of submitted documentation. Simple reimbursement claims with complete information may be resolved within a few weeks, while more complex medical claims can take longer due to provider verification and billing reviews.
Delays are more likely when documents are missing, additional clarification is required, or third parties are slow to respond. In many cases, processing pauses reflect pending information rather than disagreement over eligibility.
Responding promptly to insurer requests and follow-up questions helps reduce unnecessary back-and-forth and keeps the claim moving toward resolution.
How Can You Make the Travel Insurance Claims Process Smoother
The travel insurance claims process becomes significantly easier when preparation begins before travel. Knowing how to contact the insurer, understanding how provider networks operate, and keeping documentation organized reduces uncertainty and decision pressure during emergencies.
When an incident occurs, early communication with the insurer’s assistance team enables better coordination and clearer guidance. After treatment or a travel disruption, submitting complete documentation in a timely manner helps prevent avoidable follow-ups and delays.
Travel insurance works best when approached as an ongoing process rather than a document reviewed only after something goes wrong. Treating claims preparation as part of travel planning leads to more predictable outcomes when a claim is needed.
How Can You Avoid Claim Delays Before They Happen
The right travel insurance plan sets expectations long before a claim is needed. Coverage structure, provider network access, documentation requirements, and claims procedures vary widely between plans, and these differences matter most during medical emergencies or travel disruptions.
When purchasing travel medical insurance for yourself or for visiting family members, understanding how claims are typically handled—rather than relying only on brochures or summaries—helps reduce stress and uncertainty later.
At OnshoreKare, we help travelers and families understand how plans work in real claim situations, so expectations are clear and surprises during the claims process are minimized.
For guidance on plan selection and claims-related considerations, you can speak with the OnshoreKare team before travel.
What This Guide Does Not Cover
This guide explains how the travel insurance claims process typically works and how to reduce avoidable delays. It does not evaluate individual policy exclusions, guarantee claim outcomes, or address disputes, appeals, or legal proceedings.
Claim eligibility ultimately depends on the specific policy terms, coverage limits, and exclusions in force at the time of the incident.
Frequently Asked Questions
Who pays first in a travel insurance claim?
This depends on whether the claim is handled as a cashless or a reimbursement claim. In cashless claims, the insurer coordinates directly with the medical provider and settles eligible expenses, subject to approvals and policy limits. In reimbursement claims, the traveler pays expenses upfront and submits documents later for review and repayment. Provider network status and early notification often determine which process applies.
Can a travel insurance claim be filed while still abroad?
Yes. Most insurers allow claims to be initiated while the traveler is overseas, particularly for medical emergencies. Early notification helps with hospital coordination and documentation guidance. Final settlement may still take place after the traveler returns, once all bills and reports are available.
What happens if some claim documents are missing or incomplete?
Missing or unclear documents usually result in delays rather than immediate rejection. Insurers may request additional medical notes, itemized bills, or proof of payment before proceeding. Prompt responses and organized records help keep the claim moving forward.
How long do travel insurance claims usually take to settle?
Simple claims with complete documentation may be resolved within a few weeks. More complex medical claims can take longer due to hospital verification, third-party coordination, or clarification requests. Delays are most often linked to incomplete information rather than disputes over eligibility.
Does buying travel insurance through an advisor help with claims?
Advisors do not approve claims, but they can help explain procedures, review documentation, and assist with follow-ups. This support can be especially helpful for first-time buyers, senior travelers, or families managing claims remotely.
What should I do if the hospital asks for payment even though my policy offers cashless treatment?
Even when a policy offers cashless treatment, hospitals may request payment if approvals are pending or coordination is incomplete. In such situations, contacting the insurer’s assistance team immediately helps clarify next steps and available options. A payment request does not automatically mean the expense will not be eligible for a claim.
Can multiple bills from the same hospital be submitted under one travel insurance claim?
Yes. A single medical visit may generate multiple bills from different providers, such as doctors, laboratories, or imaging services. These bills can usually be submitted together under one claim, as long as they clearly relate to the same incident and policy period.
What happens if a claim review is taking longer than expected?
Longer review times usually indicate pending verification, missing information, or delays from third parties such as hospitals or airlines. Periods of inactivity generally reflect outstanding inputs rather than a claim decision. Responding promptly to insurer requests helps move the process forward.
Can family members help manage a travel insurance claim on behalf of the traveler?
Yes. Family members can often assist with documentation, communication, and follow-ups, particularly when the traveler is unwell or overseas. Insurers may require basic authorization or consent, depending on the situation and claim type.


